Biomarkers Are Changing Everything – A New Era in Alzheimer’s Research

Tyler Ford
June 19, 2025
Coming from a family with a history of Alzheimer’s disease, Sarah DeVos has a highly personal relationship to Alzheimer’s research. In an interview with Translating Proteomics host Andreas Huhmer, Dr. DeVos went as far as to say that, despite being asymptomatic, she knows she “…probably [has] plaque starting to form in [her] brain.” Knowing this, Dr. DeVos has devoted herself to studying Alzheimer’s in the hopes of one day developing effective treatments or even a cure.
In this blog post, we share some of the key takeaways from Dr. DeVos’ interview. As you’ll learn, new Alzheimer’s biomarkers and learnings from recently approved Alzheimer’s therapeutics are forging a new era in Alzheimer’s research that may lead to vastly improved outcomes for Alzheimer’s patients and their families.
Moving beyond post-mortem Alzheimer’s diagnosis
Until recently, Alzheimer’s was only diagnosed post-mortem. Upon examining the brains of individuals who’d shown symptoms of the disease in life, doctors could only provide a definitive diagnosis after observing amyloid plaques and tau tangles in the post-mortem brain.
As Dr. DeVos says, a post-mortem diagnosis is “obviously too late.” Recently however, researchers have developed means of visualizing amyloid plaques and tau tangles in the brains of live patients using positron emission tomography (PET). While these visualization techniques require specialized equipment and tracers, they enable far earlier diagnosis, improve patient selection for clinical trials, and provide more opportunities to monitor and learn from disease progression.
Now researchers are developing even more accessible means of measuring Alzheimer’s biomarkers. For example, in March 2025, the FDA approved a blood test for Alzheimer’s that involves the measurement of amyloid beta 1-42 as well as tau phosphorylated at threonine 217. Blood biomarkers are great because they can be measured relatively non-invasively and may enable physicians to detect Alzheimer’s at early stages. With the potential to include a variety of proteins and proteoforms, they may also give researchers and physicians more nuanced views of the molecular biology underlying Alzheimer’s in different patients.
Watch Andreas and Dr. DeVos discuss current tools and needs for Alzheimer’s diagnostics
Advances in Alzheimer’s therapeutics
Three Alzheimer’s therapeutics were recently approved. All consist of antibodies that bind to amyloid beta and cause plaque clearance. Each targets a different epitope, but all slow Alzheimer’s progression. While these drugs represent incredible progress, none of them stop Alzheimer’s, and one was discontinued in 2024.
Nonetheless, Dr. DeVos is enthusiastic about these drugs because they’re setting us on a path toward better, more personalized therapies. Indeed, she points out that, in the clinical trials leading to their approval, at least two of these drugs appeared to achieve better outcomes in patients with low levels of tau pathology. Future trials may achieve better results if patients are enrolled before tau pathology begins. In addition, combination biomarkers identifying the forms of tau, amyloid beta, and neuroinflammation present in patient brains may enable physicians to design better, more tailored therapies.
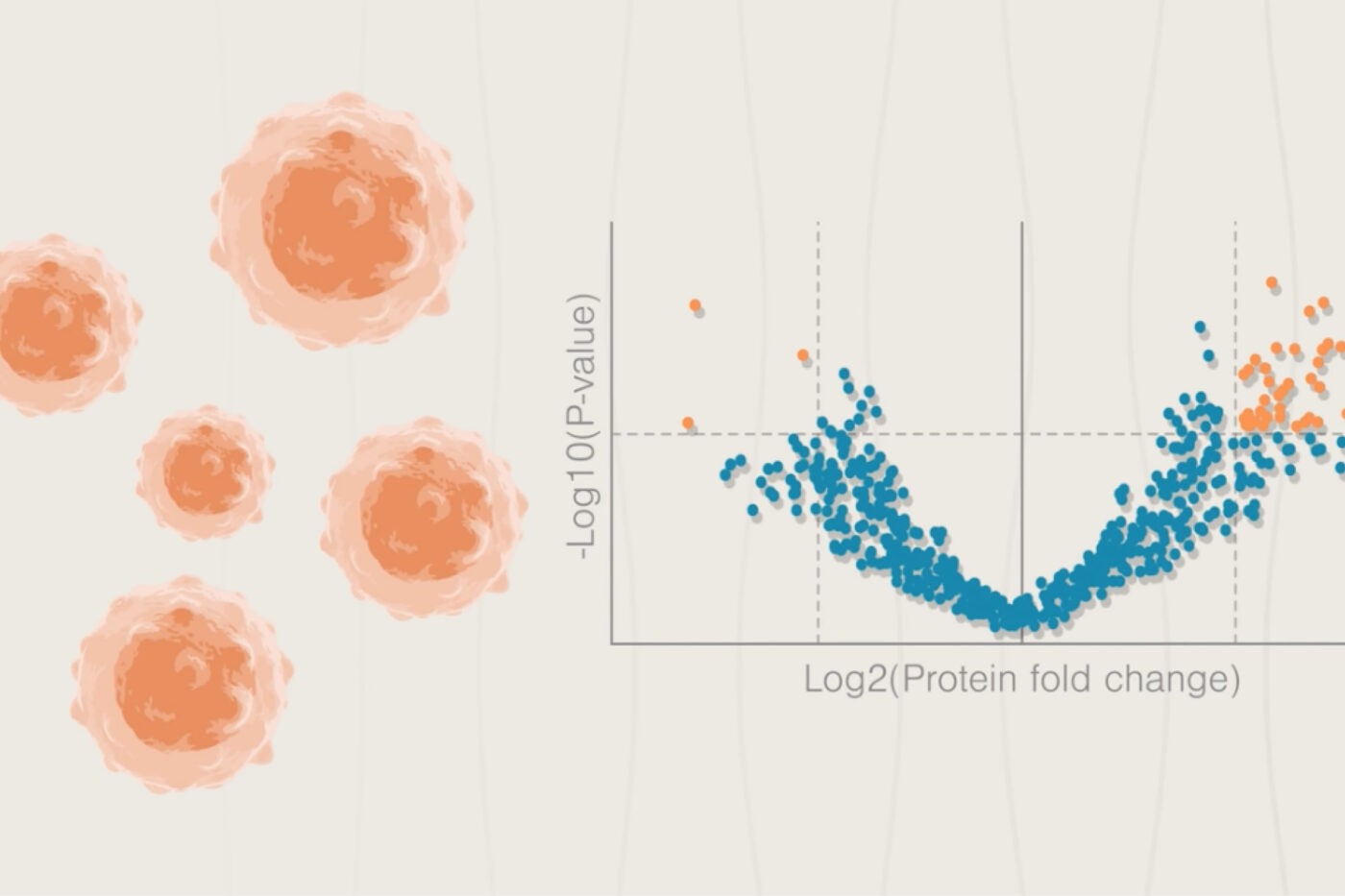
Dr. DeVos also highlights the benefits of efforts like the Dominantly Inherited Alzheimer Network (DIAN), which closely tracks molecular changes in individuals with genetic forms of Alzheimer’s. DIAN studies have been pivotal to identifying markers of disease progression. Similar studies with higher sensitivity measurements of proteins and proteoforms may provide greater granularity to our understanding of the disease and open new therapeutic avenues.
Watch Andreas and Dr. DeVos discuss recent drug approvals in the Alzheimer’s space
New approaches to Alzheimer’s disease
Throughout the interview, Dr. DeVos stresses that, as with cancer, early detection of Alzheimer’s will be the key to more effective and potentially preventative treatments. If physicians can catch patients just as their amyloid plaques begin to form, they may be able to prescribe therapies that clear these plaques and prevent progression.
In addition, Dr. DeVos suggests that it may be important to identify the form of tau responsible for disease progression. We know tau modifications like pT217 have been strongly tied to Alzheimer’s, but Dr. DeVos says she does not think it’s just one modification that makes tau pathogenic. As she eloquently states, “Anything that’s -ated, tau has it at some point.” Thus, getting a holistic view the phosphorylation, acetylation, ubiquitylation, and other modification events that create pathogenic tau proteoforms may advance efforts to develop effective biomarkers and therapies.
Finally, Andreas and Dr. DeVos discuss the importance of combining learnings from a variety of model systems and biomarker measurements across many stages of disease. By understanding what models are the best to study different stages of disease and learning more about its pathological progression, we should be able, as Andreas says, “make treatments not just early but also personalized.”
Watch Andreas and Dr. DeVos discuss how polemics can advance Alzheimer’s research
The new era of Alzheimer’s research
We are thankfully moving far beyond the time when Alzheimer’s could only be diagnosed post-mortem. The advances discussed above have come at a crucial time because, as the US population ages, Alzheimer’s cases are expected to grow in the next few decades. At Nautilus, we hope our platform can help researchers discover new and effective solutions for patients and families. As part of these efforts, we’ve developed an assay capable of measuring thousands of tau proteoforms. Find data generated using the assay here and be sure to reach out to us if you’d like to learn more.
MORE ARTICLES